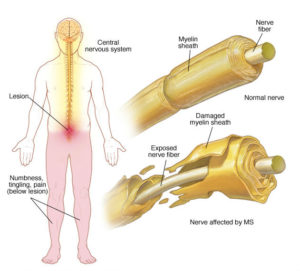
Demyelinating diseases are a group of disorders in which the myelin sheath which covers the nerves found within the brain and/or spinal cord is damaged this results in alteration of the nerve impulses resulting in neurological disorders. Damage to Meylin sheath typically occurs secondary to inflammatory process.
Multiple Sclerosis is the most common demyelinating disease. This is more common in women than men and tends to most commonly occur in young adults however it can also occur in children and the elderly. The hallmark of this disease is focal areas of myelin loss within the central nervous system (brain and/or spinal cord).
Subtypes of demyelinating disease treated at Premier Neurology and Pain Specialists:
- Multiple Sclerosis: 4 subtypes:
- Relapsing Remitting MS- most common form
- Secondary Progressive MS
- Primary Progressive MS
- Relapsing Progressive MS
Symptoms of MS are variable. Can start with eye pain or vision changes or with shooting facial pain. Patients may also experience numbness or tingling, weakness, changes in walking, inability to completely empty bladder and other presentations are possible.
Optic Neuritis
- Typically starts in adolescence after a viral infection
- Complaints of eye pain, blurry vision or even loss of vision
Transverse Myelitis
- Spinal cord inflammation resulting in demyelination after an infection or non-infectious causes.
- Sensory, motor or autonomic findings
Neuromyelitis Optica (Devic’s disease)
- Occurrence of optic neuritis involving one or both eyes with transverse myelitis
- Has tendency to spare the brain.
- More common in women
- Residual impairment is greater in Devic’s patient than MS after flare up.
Clinically isolated syndrome
- This is a monophasic syndrome that at times progresses into a chronic demyelinating disease. May present as transverse myelitis or optic neuritis
Acute Disseminated Encephalomyelitis
- Multifocal CNS inflammation that maybe monophasic but can be multiphasic caused by an autoimmune reacition after vaccination or an infection.
Diagnostic workup:
- History and physical examination
- MRI brain and spinal cord
- MRI of the optic nerves
- Visual and Auditory evoked potentials
- Somatosensory evoked potentials
- Lumbar puncture for CSF analysis
Treatment:
- Disease modifying therapies: works by slowing the progression
- Injections: I.e Copaxone ®, Rebif ®, Avenox ®
- Tablets/pills: Aubagio ®, Zeposia, Vumerity Etc
- Infusions: Ocrevus etc.
- Acute management of flare up
- High dose IV steroids
- Plasma Exchange
- Patients would require regular blood work to evaluation change in blood counts, liver function, vitamin D and calcium changes.